A quick note for readers: the things I post in this newsletter are not meant to be comprehensive. Each underlined heading is a link so you can read the information for yourself as well. I prioritize writing about things that: 1. are timely, 2. I am personally able to summarize for those who can’t spend the energy decoding on their own, and 3. are “high-yield,” as we say in medical school.
I can’t catch all the news! That’s where you come in! Please email me or DM me on Twitter if you see something you’d like included here. I want to make sure I’m addressing the biggest needs for those with chronic illness who are trying to keep up in order to advocate for themselves, as well as medical professionals who aren’t able to spend the time and energy sifting through everything each week to learn as new information comes out.
News
I haven’t kept up with it much, but it sounds like the folks who tuned in were relieved to hear some logic for once. Big deal and hopefully leads to some changes. Click on “OSHA Hearing” above to see some recordings.
Ed Yong’s latest piece is scarier than ever. The TL;DR is: climate change makes more pandemics. We can’t fight one without fighting the other.
Relatedly, this week the CDC reported the first human case of H5N1 bird flu…
In an incarcerated man in Colorado who was exposed to poultry through his work on a farm, highlighting how important it is to protect those who are incarcerated, and how dangerous conditions for them impact us all (not that that should be your reason for caring about the 2 million incarcerated people in the US)
On Wednesday, Fauci stated on PBS NewsHour that “the US is out of the pandemic phase”
…and then walked back that statement later that same day, saying "We’re really in a transitional phase, from a deceleration of the numbers into hopefully a more controlled phase and endemicity. By no means does that mean the pandemic is over.”
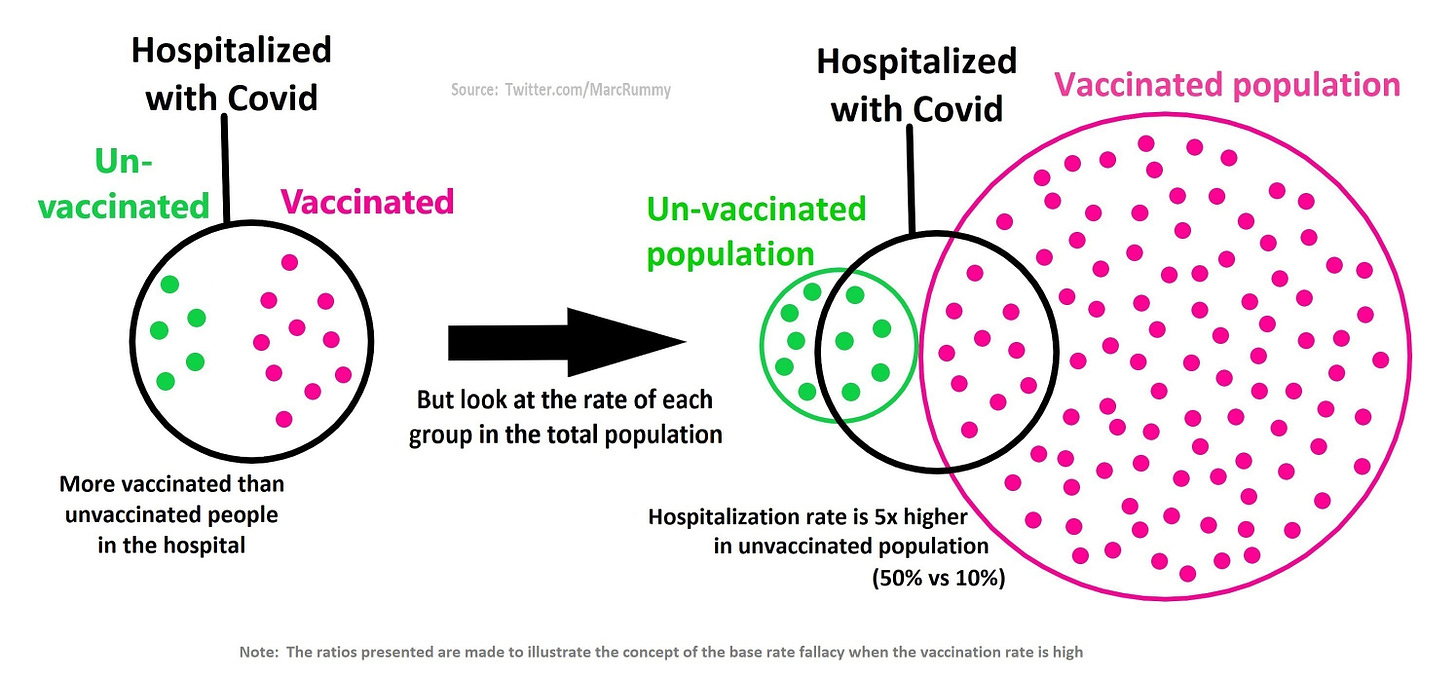
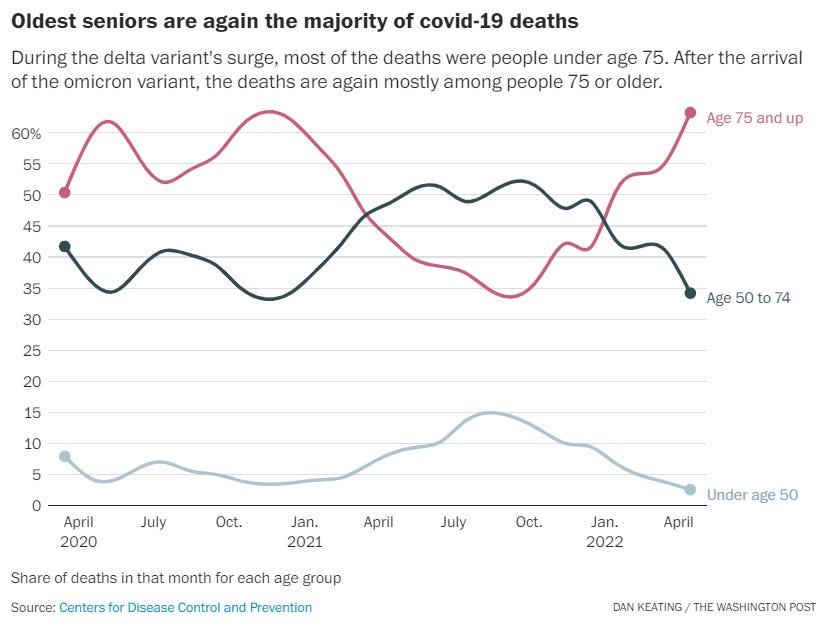
Covid deaths are no longer overwhelmingly among the unvaccinated
Arianne Bennett recalled her husband, Scott Bennett, saying, “But I’m vaxxed. But I’m vaxxed,” from the D.C. hospital bed where he struggled to fight off covid-19 this winter.
Op-Ed: Don’t pretend we’re ‘back to normal.’ Fight for cleaner air to prevent COVID
While I don’t agree with some of this (like the fact that we are at a manageable point in the pandemic), this op-ed does a great job of highlighting the need for better ventilation and general, broad protective measures (not just masks!) to ensure that the next wave of airborne illness doesn’t spread as wildly as previous ones have. Some excerpts:
We know that “transmission can happen at a distance of more than 6 feet, and infectious particles exhaled by a sick person can hang in the air for more than 15 minutes.”
The CDC, the WHO, and other major agencies have all acknowledged the role of airborne transmission since last year. But in the U.S., we’re not acting sufficiently with that knowledge.
“The public should be notified of the air quality in buildings and public transit before entering, as well as of its potential health effects such as COVID risk”
“Just as restaurants have health inspection reports with letter grades in their windows, shared indoor spaces should display their air quality ratings” to help people adjust their behavior appropriately.
Research
Characterization of Autonomic Symptom Burden in Long COVID: A Global Survey of 2,314 Adults
Note that this is a preprint, so not peer-reviewed yet.
This study included both participants who had tested positive for COVID-19 (test-confirmed) and participants who were diagnosed with COVID-19 based on clinical symptoms alone (test-unconfirmed)
Findings indicate that 67% of Long-COVID patients have moderate to severe autonomic dysfunction, which is an estimated 38 million Americans.
They also found that the levels of functional disability did NOT differ between those who had been hospitalized during their acute infection and those who were not hospitalized.
The conclusion sentence says it all: “Moderate to severe autonomic dysfunction was seen in all PASC groups in our study, independent of hospitalization status, suggesting that autonomic dysfunction is highly prevalent in the PASC population and not necessarily dependent on the severity of acute COVID illness.”
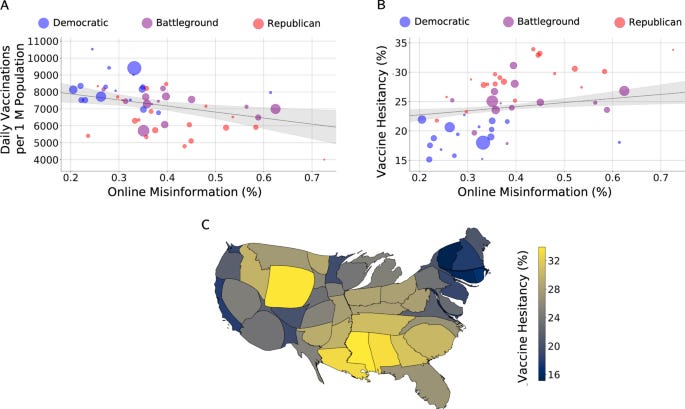
Online misinformation is linked to early COVID-19 vaccination hesitancy and refusal
This study looked at the mean percentage of vaccine-related misinformation, shared via Twitter, at the US state and county level, and compared this to rates of vaccination uptake (at the state level) and vaccine hesitancy (at state and county levels).
The most interesting finding in my opinion is: the effect of online misinformation on hesitancy is strongest across Democratic (rather than Republican) counties
This preprint went viral recently, leading some folks to conclude that mRNA vaccines are less useful than adenovirus vaccines for Covid-19.
The authors looked at randomized control trials for mRNA and adenovirus Covid vaccines, but seem to have cherry-picked a fair amount of data. There are a number of inconsistencies, including some deaths that were reported in the original studies as “unspecified” that the authors of this preprint decided to analyze as non-COVID-related, and other deaths that weren’t included at all. The TL;DR for this one is: this study is bad science. It’s not possible to aggregate the deaths from all these studies without a lot more effort — effort that these authors don’t seem to have put in. Will be interesting to see if this gets through the peer-review process.
Check out these two threads for a deeper dive: thread 1, thread 2
Note that this is a preprint, so not peer-reviewed yet.
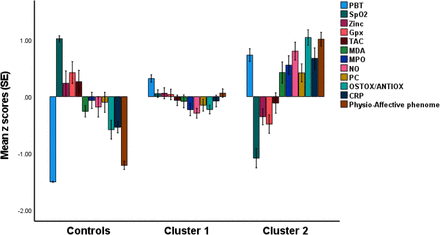
This is a combination study design—part case-control and part retrospective cohort—with 120 participants. Inclusion criteria: at least two symptoms consistent with Long COVID as per WHO guidelines, and previous diagnosis of acute COVID-19 infection. Lots of exclusion criteria.
A good thing: 1/3 of the control group (no Covid infection) had distress or adjustment symptoms as a result of lockdowns and social isolation. This is good because it helps account for confounding during analysis, since these symptoms are also seen commonly in Long-COVID patients.
31.7% of the Long COVID patients had severe abnormalities in SpO2 and body temperature, increased oxidative toxicity, and lowered antioxidant defenses.
“Long COVID is associated with immune-inflammatory processes and decreased antioxidant defenses, while a subgroup of Long COVID patients additionally exhibits increased nitric oxide production, oxidative damage to proteins and lipids with increased aldehyde formation (MDA), and immune-oxidative stress response (MPO and CRP on the graph below).”
Lots more really interesting findings that I don’t have the energy to sift through at the moment, but I’ll plan to include an update in a future newsletter if/when this passes through peer-review.
Long COVID: The Nature of Thrombotic Sequelae Determines the Necessity of Early Anticoagulation
This article summarizes the evidence for coagulation abnormalities in long COVID, with a focus on mechanisms of thrombosis. Key points:
discharged COVID-19 patients are still at risk of thrombosis
abnormal coagulation is a common manifestation in long COVID, with prolonged coagulation activation, microvascular injury, and thrombosis driving systemic damage in patients.
Impaired lung function and chronic hypoxia (due to lung changes, hypertension, embolism, and fibrosis, which are all common in long-COVID) aggravate vascular inflammation and coagulation abnormalities.
There is increasing evidence that early anticoagulation can be effective in improving outcomes.
Persistent systemic vascular inflammation and dysfunction caused by thrombosis are key factors driving various complications of long COVID.
Early prophylactic anticoagulation can prevent the release of or remove procoagulant substances, thereby protecting the vascular endothelium from damage, reducing thrombotic sequelae, and improving quality of life for long-COVID patients.
This is a retrospective study of 2,546 COVID-19 positive pediatric patients (age ≤ 21 years) who were admitted the ICU in North America.
10.8% of these pediatric patients were diagnosed with acute kidney injury. This AKI cohort had significantly higher:
length of stay at the hospital
Pediatric Index of Mortality (PIM2+3) probability of death
mortality
and needs for
airway and respiratory support
cardio-respiratory support
kidney support
vascular access
Conclusion: “Although the course of the COVID-19 virus appears milder in the pediatric population, renal complications may result, increasing the risk of disease complication and mortality.”
Here’s a link to a nice summary of this article: click for summary
Long COVID in Children and Adolescents: A Systematic Review and Meta-analyses
They used the NICE criteria to define long-COVID, which consists of both ongoing (4 to 12 weeks) and post-COVID-19 (≥12 weeks) symptoms
21 studies met the authors’ inclusion criteria and were included in this systematic review and meta-analysis
A total of 80,071 children and adolescents with Covid-19 were included, and the authors found the prevalence of long-COVID in this population to be 25.24%.
Important to use caution with this data because:
this is a preprint, and
there’s a lot of heterogeneity + lack of standardized definitions wrt published studies on long-Covid in children right now.
Regardless, though: 25% is on the higher end of the 10-30% long-Covid in adulthood stat. It’s not a number to dismiss.
Resources
While it isn’t out yet, this is a book to keep on your radar. Look for it in November!
This brilliant piece of writing would be a great read for anyone who is seeking to better understand a chronically ill loved one.
How does the phrase “getting covid is inevitable” relate to the rhinoceros?
This is just a really nice read for those of us feeling like we’re overreacting, or that our anxiety is unfounded.